What if, in people with blinding retinal disorders, one could simply introduce into the retina healthy photoreceptor cells derived in a dish from stem cells, and restore sight?
To develop a cell therapy, Beltran's team joined with groups led by John Wolfe of CHOP and Penn Vet; David Gamm at the University of Wisconsin-Madison; and Kapil Bharti at the NEI, in a consortium supported by the NEI's Audacious Goals Initiative for Regenerative Medicine. The partnership combined Beltran's team's expertise in canine models of retinal degeneration and vast experience in cell-based therapy approaches from the Wolfe, Gamm, and Bharti labs.
Photoreceptor cells, which are made up of rods and cones, constitute a layer of the outer retina critical to initiating the process of vision, whereby the energy of light transforms into an electrical signal. To function properly, they must form a connection, or synapse, with cells of the inner retina to pass along the visual information. Thus, the goal of this cell therapy is to recreate this layer and enable it to integrate with the retina's other cell types in order to relay signals from one layer to the next.
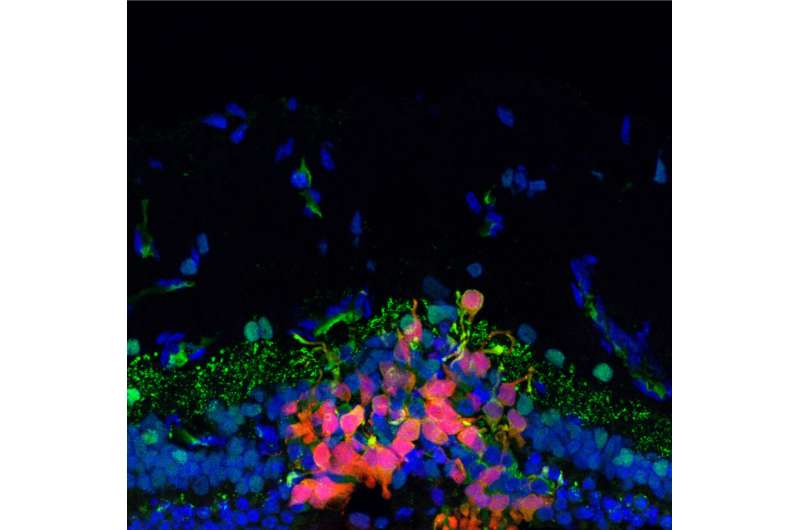
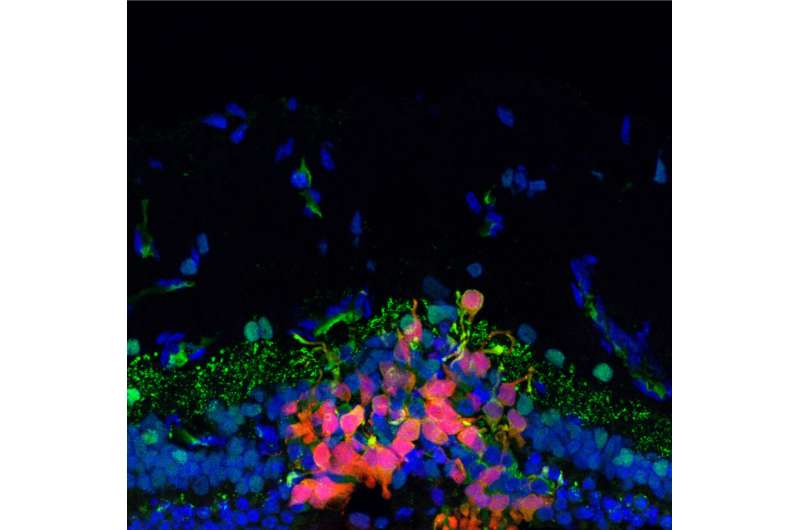
In the current work, the team used stem cell–derived precursors of human photoreceptor cells developed in the Gamm lab to serve as the basis of the cell therapy. In collaboration with the Bharti lab, they developed a new surgical approach to inject the cells, which were labeled with fluorescent markers, into the retinas of seven dogs with normal vision and three with a form of inherited retinal degeneration, then used a variety of non-invasive imaging techniques to track the cells over time.
"The use of a large animal model that undergoes a naturally occurring form of retinal degeneration and has a human-size eye was instrumental to optimize a safe and efficient surgical procedure to deliver doses of cells that could be used in patients," says Gamm.
The researchers observed that cell uptake was significantly better in the animals with retinal degeneration compared to those with normal retinas.
"What we showed was that, if you inject the cells into a normal retina that has its own photoreceptor cells, the retina is pretty much intact and serves as a physical barrier, so the introduced cells don't connect with the second-order neurons in the retina, the bipolar cells," Beltran says. "But in three dogs that were at an advanced stage of retinal degeneration, the retinal barrier was more permeable. In that environment, cells had a better ability to start moving into the correct layer of the retina."
Because the transplanted human cells could be interpreted by the dogs' immune system as foreign entities, the researchers did what would be done in other tissue transplant procedures: They gave the dogs immunosuppressive drugs. The trio of medications had been tested previously by Oliver Garden, a veterinary immunologist with Penn Vet at the time of the study, who is now dean of Louisiana State University School of Veterinary Medicine.
Indeed, while the injected cell populations declined substantially in dogs that did not receive the immune-suppressing drugs, the cell numbers dipped but then sustained in the dogs that received the cocktail.
Further characterization of the introduced cells revealed evidence of potential synapses. "We saw that yes, some are appearing to 'shake hands' with those second-order neurons," Beltran says. "There appeared to be contact."
The next stage for this project will be to continue optimizing the therapy, and then test whether there is a functional response—in other words, improved vision—in its recipients.
More information: Ana Ripolles-Garcia et al, Systemic immunosuppression promotes survival and integration of subretinally implanted human ESC-derived photoreceptor precursors in dogs,
Stem Cell Reports (2022).
DOI: 10.1016/j.stemcr.2022.06.009
Citation: Progress toward a stem cell–based therapy for blindness (2022, July 29) retrieved 29 July 2022 from https://medicalxpress.com/news/2022-07-stem-cellbased-therapy.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without the written permission. The content is provided for information purposes only.








 User Center
User Center My Training Class
My Training Class Feedback
Feedback












Comments
Something to say?
Log in or Sign up for free