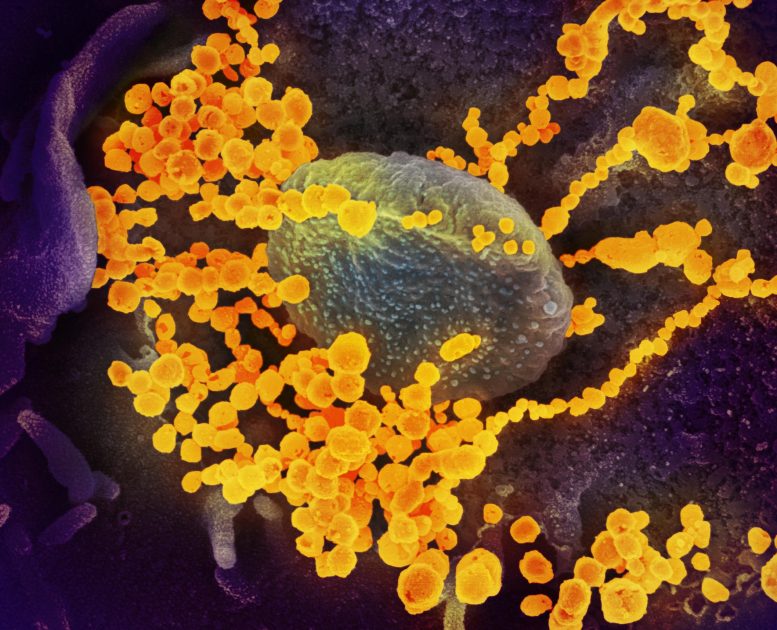
This scanning electron microscope image shows SARS-CoV-2 (round gold objects) emerging from the surface of cells cultured in the lab. SARS-CoV-2, also known as 2019-nCoV, is the virus that causes COVID-19. The virus shown was isolated from a patient in the U.S. Credit: NIAID-RML
More than 300 scientists and clinicians from the federal government, industry and academia published a report of their conclusions and recommendations on COVID-19 serology studies online in Immunity. The group gathered for an online workshop in May to discuss the role of serology testing in understanding and responding to the COVID-19 public health crisis and to explore strategies to address key scientific knowledge opportunities and gaps in the emerging field. Serology tests for COVID-19 are designed to detect antibodies against SARS-CoV-2, the virus that causes COVID-19. While such tests do not diagnose active infection, they can indicate prior infection with SARS-CoV-2 that may have been missed because a person did not experience significant symptoms or access testing while infected.
The COVID-19 Serology Studies workshop was convened by an interagency working group comprised of experts from the U.S. Department of Health and Human Services—including scientists at the National Institute of Allergy and Infectious Diseases (NIAID), the National Cancer Institute (NCI), and the National Heart, Lung and Blood Institute (NHLBI), parts of the National Institutes of Health, as well as the Centers for Disease Control and Prevention and the Biomedical Advanced Research and Development Authority—and the Department of Defense. Attendees assessed efforts to better understand the implications of serology test results, to produce and validate test kits, and to quantify undetected cases of SARS-CoV-2 infection.
Attendees recommended that additional research is needed to determine if and to what extent a positive antibody test means a person may be protected from reinfection with SARS-CoV-2. Attendees emphasized that until such data is available, serology tests should not be used as a stand-alone tool to make decisions about personal safety related to SARS-CoV-2 exposure. Researchers are now pursuing studies in humans and in animal models to better understand SARS-CoV-2 immunity. Attendees noted that such understanding could help identify optimal donors of convalescent plasma that potentially could be used to help treat those with severe COVID-19.
Researchers from NCI reviewed progress in their effort to independently validate SARS-CoV-2 serology testson behalf of the U.S. Food and Drug Administration. Attendees also proposed strategies to expand the accuracy and capacity of these tests to distinguish between naturally acquired and vaccine-induced antibodies, which will be critical to evaluating COVID-19 vaccine candidates.
Both community-based and large-scale serology surveillance efforts—such as the RESPONSE study sponsored by NIAID and NHLBI—are collecting critical data to improve epidemiological models and inform public health decision-making. Ideally, attendees noted, federal partners will expand this activity to establish an interactive serological database that will help public health officials monitor and quickly respond to changes in SARS-CoV-2 infection patterns.
Reference: “The COVID-19 Serology Studies Workshop: Recommendations and Challenges” by Andrea M. Lerner, Robert W. Eisinger, Douglas R. Lowy, Lyle R. Petersen, RosemaryHumes, Matthew Hepburn and M. Cristina Cassetti, Immunity.
DOI: 10.1016/j.immuni.2020.06.012








 User Center
User Center My Training Class
My Training Class Feedback
Feedback












Comments
Something to say?
Log in or Sign up for free